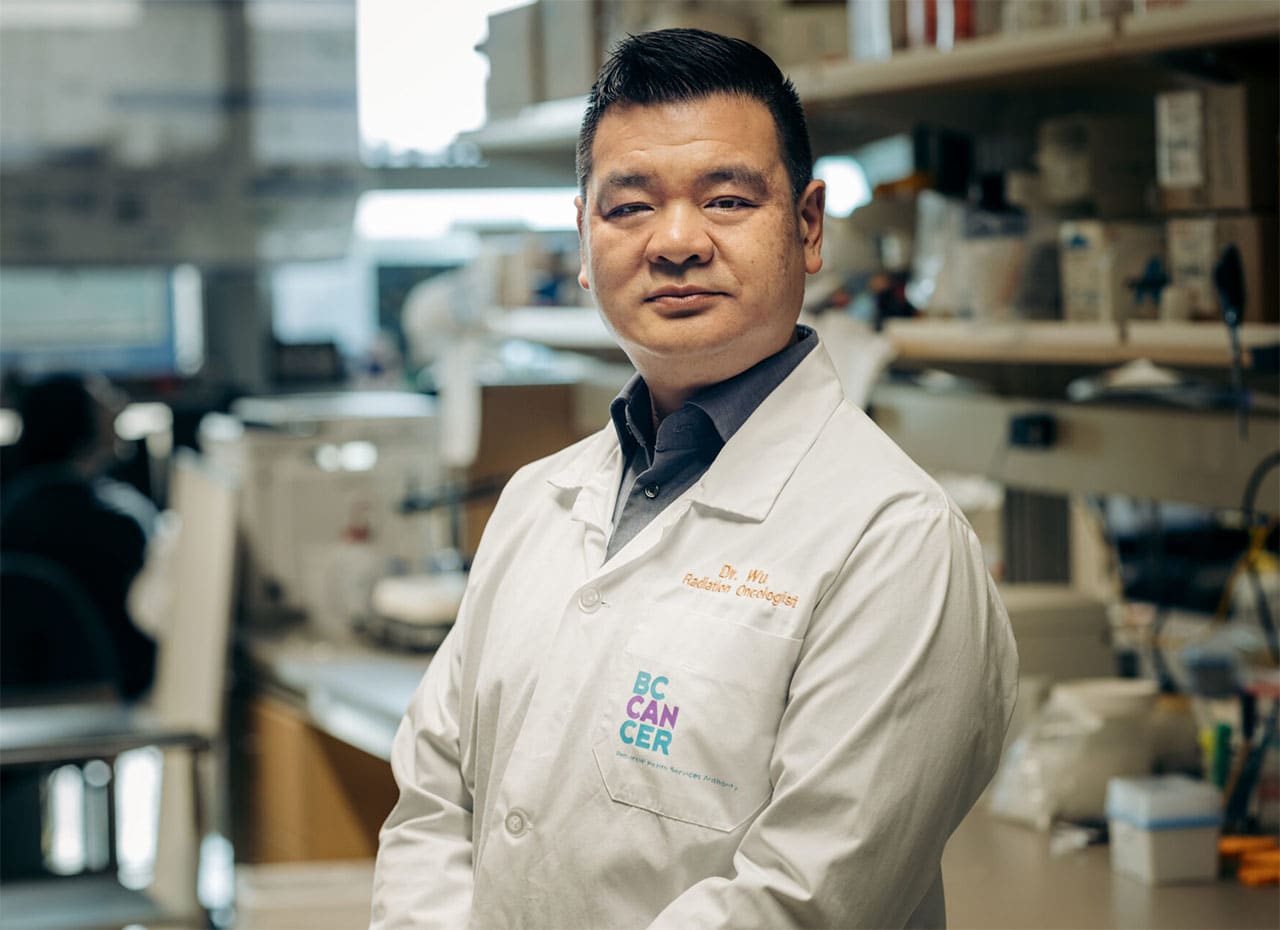
Dr. Jonn Wu: Looking Beyond a Cure to Increase Quality of Life for Head and Neck Cancer Patients
December 20, 2023
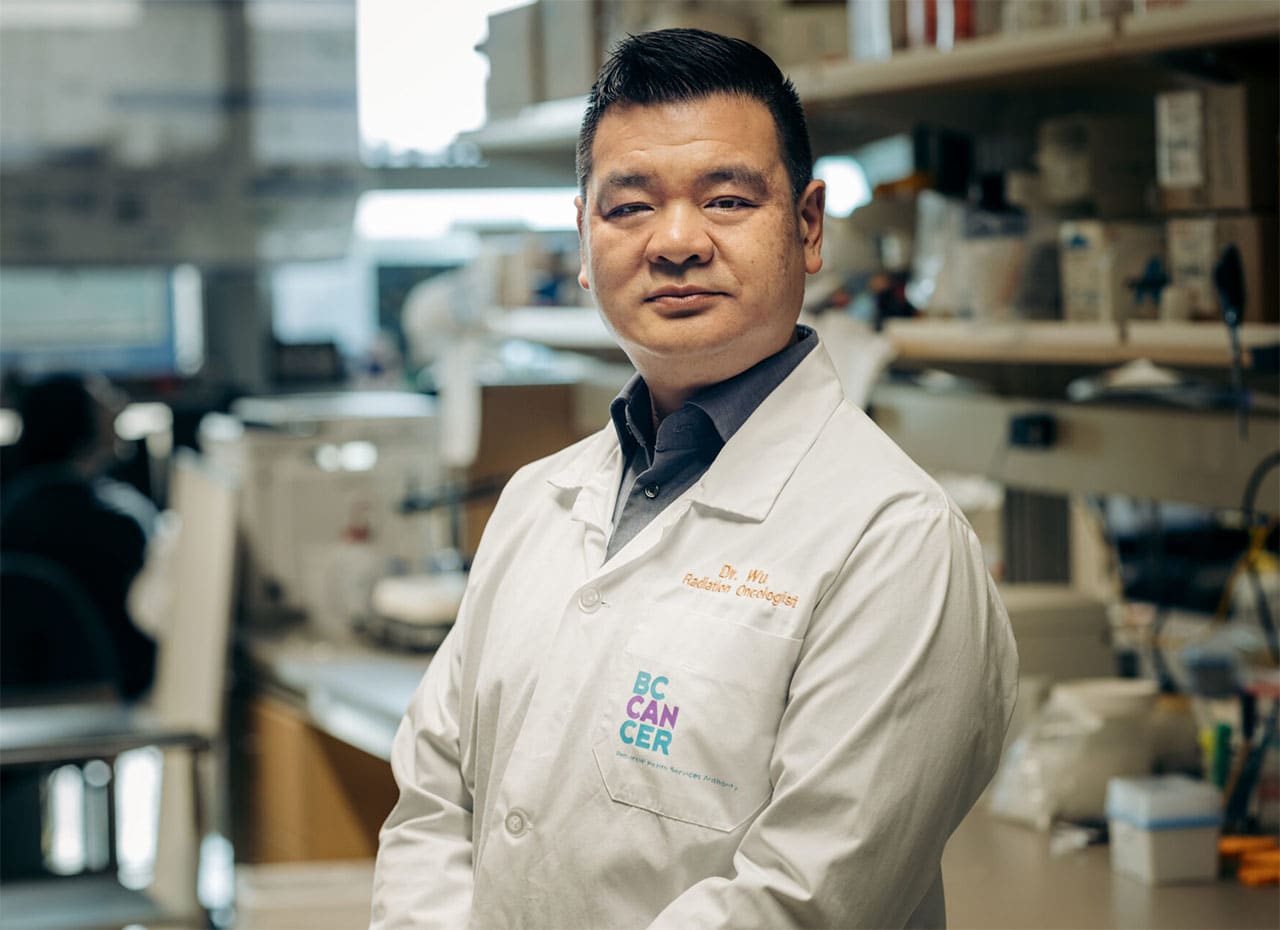
“If time travel was real and someone went back to 1993 to the start of my career in radiation therapy and told me how much it would change in 30 years, I would call them crazy,” laughs Dr. Jonn Wu.
Even more unbelievable to Dr. Wu — who had just graduated from the University of Alberta in the early ’90s — would be the knowledge that he would help develop a new cutting-edge way of delivering focused radiation which would become standard care for throat cancer patients in B.C.
Born in Taiwan, but raised in Burnaby, Dr. Wu did his medical, oncology and radiation training in Alberta. But it was at the University of Washington in Seattle that he was introduced to different head and neck cancer treatment protocols and helped develop intensity modulated radiotherapy (IMRT), a more precise radiation therapy that spares healthy tissue and limits adverse side effects.
The plan, and the stipulation of the scholarship that took him to the U.S., was that Dr. Wu would bring these new skills back to Edmonton. Instead, after funding fell through from the University of Alberta, BC Cancer snapped him up within weeks of receiving the application he sent out merely as a back-up.
“Back then only a handful of hospitals were doing IMRT in the U.S. Vancouver really wanted that technology, so they were excited to hire me.”
Attracted by the provincial structure at BC Cancer, which ensures patients across the province are offered the same treatment, Dr. Wu accepted a position as a radiation oncologist in Vancouver in 1999. Together, with a team of dedicated medical physicists, they implemented one of the first IMRT systems in Canada.
Using Population-Based Care to Create Better Outcomes and Reduce Side Effects
That consistency in care across B.C. — which is not available in other parts of Canada and the U.S. where cancer centres operate independently and don’t share patient data — has enabled Dr. Wu and BC Cancer oncologists Drs. Cheryl Ho and Janessa Laskin to create the Outcomes and Surveillance Integration System (OaSIS). This unique-to-B.C. software platform gathers and tracks patient information from diagnosis through treatment and into survivorship for lung and head and neck cancers.
“OaSIS helps us answer questions such as: How do I know that the treatments we offer our patients actually work? What are the cure rates? Have treatments and outcomes improved over time? What kind of side effects do our patients experience?”
This wealth of information not only informs more precise and improved treatment options for patients, it also helps change practice to reduce harmful side effects. This is particularly relevant in oral and head and neck cancers where radiation can damage the saliva glands and result in permanent and debilitating side effects such as dry mouth, impaired taste, difficulty swallowing and tooth decay.
The biological modelling that helped write the rules, now used around the world, on how to protect salivary glands by limiting radiotherapy doses, was based on this kind of access to patient data, says Dr. Wu.
“Twenty years ago it was a luxury to think about the side effects of radiation. In the ’90s I would warn patients that they would lose their saliva which impacts their ability to swallow, speak and protect their teeth. There was nothing we could do about it.”
In 2007, Dr. Allan Hovan, the provincial practice leader for oral oncology/dentistry at BC Cancer, brought the idea of measuring saliva output in patients before and after radiation to Dr. Wu. Together, they used this data to refine radiation volume to help preserve saliva production in patients. More recently, a PHD student of Dr. Wu’s (Dr. Hal Clark) identified a “magical area” in the parotid gland that could be even more game-changing, he says —“If we can protect this certain area, we might be able to protect some of a patient’s saliva.”
Donors are Making a Difference
As innovative treatments improve outcomes and patients are living longer with this disease, it’s even more important to focus on reducing adverse side effects — and philanthropy is crucial to this work.
“I rely heavily on donor dollars for much of my research. For setting up OaSis (the data from which we’ve published over 30 papers) and to fund the work of my grad students and our salivary gland research,” says Dr. Wu of the need for investment in head and neck cancers, a disease that typically doesn’t get a lot of airtime.
“There’s a misnomer that these cancers are all due to smoking and alcohol use. They’re not.” More recently, cancers of the throat, tongue and tonsils have been linked to human papillomavirus (HPV), a common sexually transmitted disease which 75% of Canadians will contract.
“When I first started out in radiation oncology, we would blast the entire neck with a beam of radiation from left to right. We’ve come a long way since then in providing more precise treatment,” says Dr. Wu.
But unfortunately there’s still a need to warn patients about possible side effects, such as trouble speaking or a temporary feeding tube after radiation. “What kind of quality of life is that?” asks Dr. Wu. “If we can improve on that, it’s definitely something we need to do.”
Transform the Future of Cancer Care
Help expand access, accelerate treatment and improve outcomes for patients across B.C.
Donate Today

