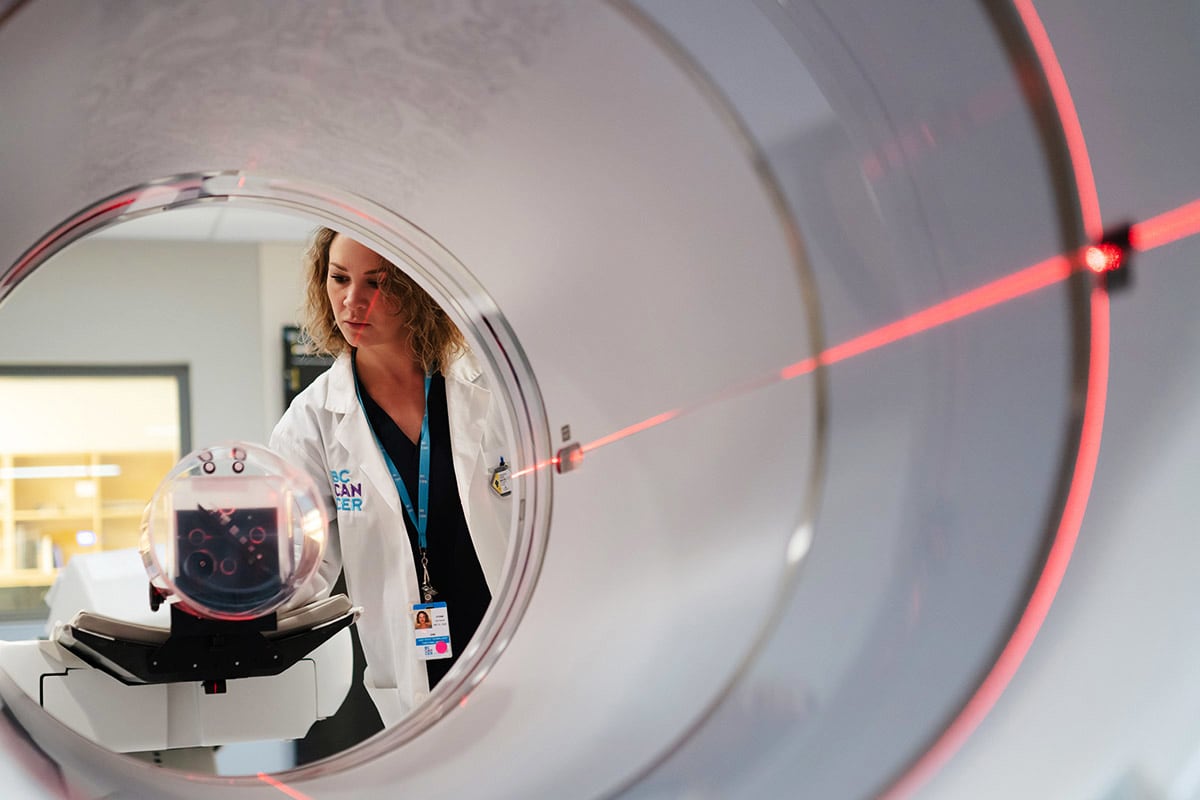
Dr. Lily Proctor: On the Road to Erasing Cervical Cancer
January 12, 2024
Found in BC Cancer - Vancouver, Cervical Cancer, General
B.C. is the first province in Canada to establish a new cervix self-screening option that will increase access to life-saving cervical cancer screening and provide a more equitable, accurate, comfortable and convenient way to test. A giant step towards the goal of eliminating the disease within ten years, it’s an initiative BC Cancer’s Dr. Lily Proctor and her team have been working on for decades.

This year, an estimated 200 women in B.C., mostly under age 50, will be diagnosed with cervical cancer and 60 will die from the disease. This, and the fact that late-stage cervical cancer cases are on the rise, is unacceptable, says BC Cancer gynecologic surgical oncologist Dr. Lily Proctor — as not only is cervical cancer highly treatable when caught early, it’s also almost entirely preventable.
In 2020, the World Health Organization approved a strategy for eliminating cervical cancer completely and Canada has pledged to meet that goal by 2040. Dr. Proctor is leading the charge in B.C.
After a fellowship in gynecologic oncology at UBC, she received a Master in Clinical Epidemiology and Public Health at Harvard before returning home to Vancouver where she’s now BC Cancer’s Cervical Cancer Colposcopy lead and the medical director of B.C.’s Cervical Cancer Screening Program.
“I had a strong desire to come back and serve the women of this province,” she says of her work focusing on cervical cancer, which unfortunately is more common among people with lower incomes, living in rural or remote areas, and in recent immigrants, First Nations, Inuit and Métis.
“Cervical cancer is essentially a disease of inequity — patients who are unable to attend screening due to personal, physical or cultural barriers are most vulnerable. If they’re not being screened, we’re not finding the precancer in its early asymptomatic phase when it can be cured with a simple procedure.”
Screening via the traditional Pap test, in which cells from the cervix are collected by a health care provider and tested in a lab, requires a pelvic examination and this can be challenging for patients with history of trauma (physical or sexual abuse) or people in the LGBTQIA2S+ community who may be uncomfortable undergoing the procedure, says Dr. Proctor.
People in Northern B.C., who have less access to health care (as well as 25% of the province who don’t have a primary care provider) are also at risk. As are immigrants due to language, education and cultural barriers that inhibit their ability to undergo life-saving screening.
The BC Cancer Foundation funded a program in the Fraser Valley to help understand how to improve screening uptake in women in the South Asian community, who fall well behind the general population.
“This information was really important and valuable to inform a variety of approaches we can use to improve screening coverage,” says Dr. Proctor, including the Province’s recent announcement to offer women or individuals from 25 to 69 with a cervix the choice to self-test at home for the human papillomavirus (HPV), the leading cause of cervical cancer.

HPV is a common sexually transmitted virus (which more than 75% of Canadians will contract) that usually goes away on its own. However, persistent infections can cause abnormal cells to develop which can lead to cervical cancer.
While Pap tests detect changes to the cervix caused by HPV, testing for the virus, before cell changes have occurred, identifies people at risk for cervical cancer earlier and better, says Dr. Proctor.
In 2021, BC Cancer launched a cervical screening pilot project in which self-swab kits were mailed to 67,000 individuals on the Sunshine Coast and on Central Vancouver Island. At the end of January 2024, Dr. Proctor’s team are commencing a province-wide roll out of the program, with plans to transition to HPV testing as a primary screening method over the next three years.
“B.C. is basically leading the way. We’re one of only several jurisdictions worldwide and the first in Canada to offer people the choice of how they want to be screened. And by allowing patients to choose, by making testing more accessible, equitable and comfortable, we are already showing that we can increase coverage in people who have never been screened or who are under screened by up to 20%.”
BC Cancer has long been at the forefront of cervical cancer prevention, says Dr. Proctor. “We launched the first population-based cervical screening program almost 70 years ago. We have a long history of offering really high-level care in this field, and this latest move to a clearly superior method of cervical cancer screening is continuing on that path.”
For Dr. Proctor and her team this is a pivotal moment in advancing cancer care in B.C.
“We’re already hearing, almost weekly, from patients who took part in the pilot project who say they didn’t have a family doctor, or they couldn’t take time off work to go and get screened. But after seeing a poster on a bus or an ad on social media for self screening, they called or emailed and received a prepaid envelope with a test they did in two minutes. As a result, they found an early cancer, are having surgery and are being cured. It’s going to be life changing for a lot of people.”
Help BC Cancer experts provide a life beyond cancer for patients across the province, donate today.